Limb-girdle muscular dystrophy 2A/R1 (LGMD 2A/R1)
Quick Search
- Summary
- Synonyms and Classifications
- Symptoms
- Disability Impacts
- Cause and Inheritance
- Diagnosis
- Treatment
- Clinical Care Team
- Clinical Care Guidelines
- Emergency Management
- Research
- Rare Disease Organisation(s)
- Lived Experience
- Support Services and Resources
- Mental Health
- Other Information
- Useful Links for Healthcare Professionals
Summary
Limb-girdle muscular dystrophy 2A/R1 (LGMD 2A/R1) is one of the more common types of limb-girdle muscular dystrophy (LGMD).1 LGMD 2A/R1 is caused by genetic changes (variants) in the CAPN3 gene.1 Conditions caused by CAPN3 gene variants are also known as calpainopathy.1,2 LGMD 2A/R1 is an autosomal recessive condition, which is represented by the letter ‘R’ (previously classified as Type 2).1,3,4
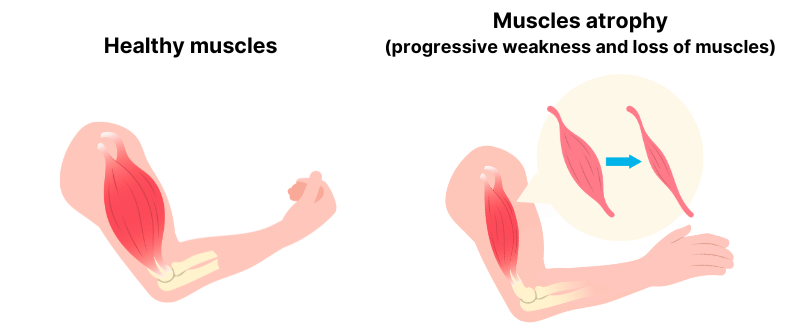
LGMD 2A/R1 is characterised by progressive weakness and loss (wasting/atrophy) of the muscles closest to the centre of the body (the proximal muscles), mainly affecting the hips and shoulders.1 This may gradually affect mobility and result in loss of ability to walk.1 There is usually no effect on heart (cardiac) muscles.1,2 The symptoms of LGMD 2A/R1 may appear during childhood or in adulthood, with reported onset of symptoms between 2-40 years.2
Synonyms and Classifications
Synonyms: Calpain-3-related limb-girdle muscular dystrophy R1; autosomal recessive limb-girdle muscular dystrophy type 2A; Calpain-3-related LGMD R1; LGMD type 2A; LGMD2A; limb-girdle muscular dystrophy due to calpain deficiency; limb-girdle muscular dystrophy type 2A; pelvofemoral muscular dystrophy; primary calpainopathy.1
Universal rare disease classifications provide a common language for recording, reporting and monitoring diseases. Please visit the Rare Disease Classifications page for more information about these internationally recognised classifications.
Symptoms
LGMD 2A/R1 mainly involves progressive weakness and loss (wasting/atrophy) of the hip and shoulder muscles.1 The weakness tends to be symmetrical (on both sides)1,2 and often affects the ability to walk, resulting in a waddling gait and difficulties in climbing stairs or getting up from a sitting position.1,2 It may progress to complete loss of ability to walk and use of a wheelchair may be required.3
Other symptoms may include abnormal protrusion of the shoulder blades (scapular winging), abnormally large calf muscles (calf pseudo-hypertrophy), shortening of muscles (contractures) and muscle pain.2,3
Please speak to your medical team to learn more about the symptoms for LGMD 2A/R1.
Disability Impacts
Rare diseases are often serious and progressive, exhibiting a high degree of symptom complexity, leading to significant disability. Majority of the estimated two million Australians living with a rare disease meet the Australian Government’s definition for disability (in accordance to the Australian Public Service Commission and Australian Bureau of Statistics), and many experience severe and permanent disability impacts. If you or someone you care for is experiencing disability-related impacts from a rare condition, please speak with a health or disability professional for advice. Information about relevant disability support can be found at the RARE Portal’s Disability Support Information page.
Cause and Inheritance
LGMD 2A/R1 is a genetic condition. It is caused by disease-causing genetic changes (variants) in the CAPN3 gene.
All individuals have two copies (alleles) of the CAPN3 gene – one on each chromosome that is inherited from each parent. LGMD 2A/R1 is an autosomal recessive condition, which means both copies of CAPN3 gene must have the disease-causing genetic variants.1,3
Individuals with the genetic variant in only one copy are unaffected but will be a carrier and may pass on that variant to their children. If both parents are carriers (each have a copy of the disease-causing variant), there is a 25% chance the child will inherit both disease-causing variants and have LGMD 2A/R1. More information on autosomal recessive inheritance pattern can be found at Centre for Genetics Education: Autosomal recessive inheritance.
If you would like to learn more about the inheritance and impact of this condition, please ask your doctor for a referral to a genetic counsellor. Genetic counsellors are qualified allied health professionals who can provide information and support regarding genetic conditions and testing. More information about genetic counselling can be found at:
- Information on Genetic Services
- The National and State Services pages underneath the ‘Genetic Counselling’ sections listed
Diagnosis
Diagnosis of LGMD 2A/R1 may be based on clinical examination, muscle biopsies, blood tests and genetic testing.1
Elevated serum creatine kinase (CK) concentration (hyperCKemia) is often observed in children or young individuals, however the concentration may decrease with disease progression and muscle loss (wasting/atrophy).1,2
Please speak to your medical team to learn more about the available diagnostic pathways for LGMD 2A/R1.
Treatment
There is currently no curative treatment for LGMD 2A/R1. Treatment is targeted at managing symptoms (symptomatic management) and involves a multidisciplinary care team. This may include physiotherapy and occupational therapy, assistive equipment, mobility and medical aids.2 Information on equipment and assistive technology can be found at The Loop – Your Neuromuscular Resource Hub: Equipment.
Please speak to your medical team to learn more about the possible treatment or management options for your condition. Treatment will depend on an individual’s specific condition and symptoms. It is also important to stay connected to your medical team so that you can be made aware of any upcoming clinical trial opportunities.
Clinical Care Team
Clinical care for rare diseases often involves a multidisciplinary team of medical, care and support professionals. Please note that the information provided here is as a guide and that RVA does not necessarily monitor or endorse specific clinics or health experts.
Healthcare professionals involved in the treatment of LGMD 2A/R1 may include general practitioners (GP), geneticists, neurologists, physiotherapists and rehabilitation specialists.1 The need for different healthcare professionals may change over a person’s lifetime and extend beyond those listed here.
The Loop – Your Neuromuscular Resource Hub: NMC Clinics lists available specialist clinics provide care and support for children and adults living with certain neuromuscular conditions across Australia.
Clinical Care Guidelines
We are not aware of any clinical care guidelines for LGMD 2A/R1 in Australia. If you know of any relevant care guidelines, please let us know via the Contribute page.
The following guidance is available from international experts outside Australia; however, there may be information that is not relevant or applicable to the Australian context, and may not be up to date:
229th ENMC international workshop: Limb girdle muscular dystrophies – Nomenclature and reformed classification (Naarden, the Netherlands, 17–19 March 2017) reports on a consensus on an updated nomenclature and classification for LGMD.
Emergency Management
Individuals living with rare diseases may have complex medical issues and disabilities, which are not always visible. It is often useful to refer to their medical history as well as personal information such as a medical card, doctor’s letter, or if available, a rare disease passport, for relevant information.
It is important for individuals to inform all healthcare providers of their LGMD diagnosis when presented at the emergency department/services.
Research
The Australian Neuromuscular Disease Registry is an Australian-wide registry that collects information about individuals with certain neuromuscular conditions, including limb-girdle muscular dystrophy (LGMD). The registry collects important medical information from adult and child patients across the country to improve the understanding of neuromuscular disease and accelerate the development of new therapies.
There are specific considerations around participating in rare disease research, including clinical trials. It is important to be mindful of issues such as data privacy, research ethics, consent and differences in research regulations between Australia and other countries.
If you are interested in finding clinical trials for your condition, please visit the following websites; however, there may not be any clinical trials available:
It is best to discuss your interest in any clinical trials with your medical team to determine suitability and eligibility.
Please note that RVA does not necessarily monitor or endorse each group/organisation’s operational governance and activities.
Rare Disease Organisation(s)
Australian Organisation:
Daniel Ferguson LGMD Foundation
Website: https://www.dffoundation.com.au/
Daniel Ferguson LGMD Foundation aims to support those living with all types of LGMD by improving their quality of life, increasing community awareness of the disorder and funding much-needed research into this disease for which no cure exists.
Please note that RVA does not monitor or endorse each group/organisation’s operational governance and activities. When engaging with a group, please consider the information on the RARE Portal’s Finding Helpful Peer and Community Supports page.
Lived Experience
LGMD 2A/R1 varies between individuals, and each person’s experience is unique.
If you would like to share your personal story with RVA, please visit the Rare Voices Australia: Share Your Story page. RVA will consider your story for publishing on our website and inclusion on the RARE Portal.
Support Services and Resources
Daniel Ferguson LGMD Foundation: Peer Support has information about peer support relevant for individuals living with LGMD.
For information on available government and social services that provide support for individuals with a rare disease, please visit the National and State Services pages.
Mental Health
People living with a rare disease, including families and carers, often face unique challenges such as diagnostic delays, misdiagnoses, limited treatment options, and limited access to rare disease specialists and support. These challenges may impact people’s emotional wellbeing and quality of life. Many people find it helpful to seek mental health and wellbeing support to cope with ongoing stress and uncertainty. Connecting with people who have shared experiences through a support group may also be helpful. Information about relevant mental health and wellbeing support can be found at:
- Mental Health and Wellbeing Support for Australians Living with a Rare Disease
- The National and State Services pages underneath the ‘Mental Health’ sections listed
Other Information
Further information relevant to LGMD 2A/R1 can be found at:
Useful Links for Healthcare Professionals
- Orphanet: Calpain 3 related limb girdle muscular dystrophy R1
- Online Mendelian Inheritance in Man, OMIM:® #253600 – Muscular dystrophy, limb-girdle, autosomal recessive 1; LGMDR1
- 229th ENMC international workshop: Limb girdle muscular dystrophies – Nomenclature and reformed classification (Naarden, the Netherlands, 17–19 March 2017)
References
- Genetic and Rare Diseases (GARD) Information Center. Calpain-3-related limb-girdle muscular dystrophy R1. Accessed 16 November 2023. https://rarediseases.info.nih.gov/diseases/1057/calpain-3-related-limb-girdle-muscular-dystrophy-r1
- Angelini, C. Calpainopathy. 2005. Updated 1 December 2022. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. Gene Reviews® [Internet]. Seattle, University of Washington; 1993- . Accessed 16 November 2023. https://www.ncbi.nlm.nih.gov/books/NBK1313/
- Online Mendelian Inheritance in Man, OMIM®. Johns Hopkins University, Baltimore, MD.#253600 – Muscular dystrophy, Limb-girdle, autosomal recessive 1; LGMDR1.Accessed 16 November 2023. https://www.omim.org/entry/253600
- Straub V, Murphy A, Udd B. 229th ENMC international workshop: Limb girdle muscular dystrophies – Nomenclature and reformed classification Naarden, the Netherlands, 17-19 March 2017. Neuromuscul. Disord. 2018;28(8):702-710. https://doi.org/10.1016/j.nmd.2018.05.007
Contributors
This page has been co-developed by Rare Voices Australia (RVA)’s RARE Portal team in consultation with Daniel Ferguson LGMD Foundation.
If you are aware of any additional information that may benefit stakeholders with an interest in this page, or if you notice any broken links or inaccurate information, please let us know via the Contribute page.

