Idiopathic multicentric Castleman disease (iMCD)
Quick Search
- Summary
- Synonyms and Classifications
- Symptoms
- Disability Impacts
- Cause and Inheritance
- Diagnosis
- Treatment
- Clinical Care Team
- Clinical Care Guidelines
- Emergency Management
- Research
- Rare Disease Organisation(s)
- Lived Experience
- Support Services and Resources
- Mental Health
- Other Information
- Useful Links for Healthcare Professionals
Summary
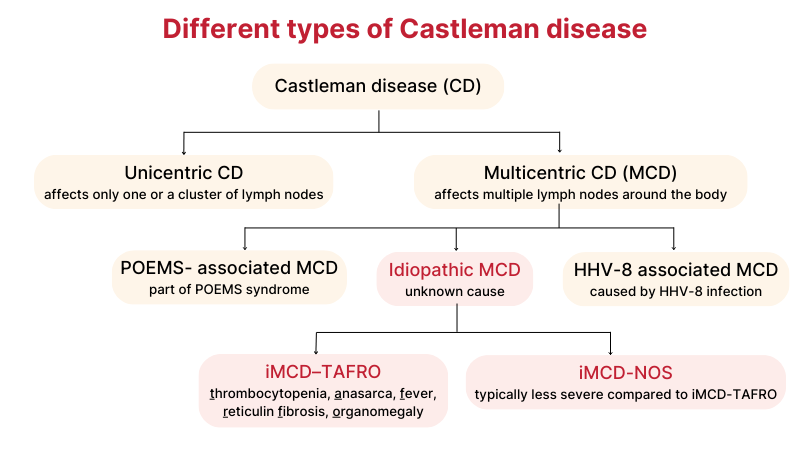
Idiopathic multicentric Castleman disease (iMCD) is a type of Castleman disease where multiple lymph nodes throughout the body become enlarged and overactive, for an unknown reason.1-3 Lymph nodes are part of the immune system and are the home base of immune cells. There are hundreds of lymph nodes in the human body. The overactive lymph nodes result in an overproduction of immune cells which can cause inflammation and damage tissues and organs throughout the body.
iMCD can be split into two subtypes depending on the symptoms present:2,4,5
- Idiopathic multicentric Castleman disease-TAFRO (iMCD–TAFRO) – characterised by the presence of thrombocytopenia (unusually low platelet count), anasarca (swelling of multiple tissues or organs), fever, reticulin fibrosis or myelofibrosis (bone marrow disease or cancer) and organomegaly (enlargement of any organs)
- Idiopathic multicentric Castleman disease-not otherwise specified (iMCD-NOS) – individuals typically have less severe symptoms and complications compared to iMCD-TAFRO
Below are other types of Castleman disease which have some overlapping symptoms with iMCD but different complications, causes, and treatment methods:
- Unicentric Castleman disease (UCD) – only involves one or one group of lymph nodes
- HHV-8-associated multicentric Castleman disease (HHV-8+MCD) – affects multiple lymph nodes, similar to iMCD but is caused by Human herpesvirus 8 (HHV-8) infection
- Castleman disease can also occur as a part of POEMS syndrome and is known as POEMS-associated multicentric Castleman disease (POEMS-MCD)
Synonyms and Classifications
Synonyms: HHV-8-negative multicentric Castleman disease, HHV-8-MCD, Human herpesvirus-8-negative multicentric Castleman disease, Castleman Disease, CD, multicentric Castleman disease, MCD, angiofollicular lymph node hyperplasia, angiomatous lymphoid, angiofollicular ganglionic hyperplasia, Castleman tumour, giant benign lymphoma, giant lymph node hyperplasia, hamartoma of the lymphatics.1,3
Universal rare disease classifications provide a common language for recording, reporting and monitoring diseases. Please visit the Rare Disease Classifications page for more information about these internationally recognised classifications.
ORPHA:570431 Idiopathic Multicentric Castleman Disease
ICD-11: 4B2Y Other specified disorders involving the immune system
Symptoms
The signs of iMCD can have a slow and subtle onset or be sudden and life threatening. The most common symptoms of iMCD include:1,2,6,7
- enlarged lymph nodes/lumps under the skin in more than one place
- flu-like symptoms which may include aches, pains, tiredness, night sweats, weight loss, appetite loss, or nausea
- spotted red or purple skin rash (cherry hemangioma or violaceous papules)
- swelling or enlargement of any part of the abdomen or organs (oedema/ascites)
- tingling or numbness in the hands or feet (peripheral neuropathy)
- difficulty breathing
iMCD can progress to multi-system organ failure and involve varying symptoms related to the specific organs impacted.1,2,6,7
There are two subtypes of iMCD:
- Idiopathic multicentric Castleman disease-TAFRO (iMDC–TAFRO)
Some people with iMCD also experience acute episodes of some of the following 5 symptoms: thrombocytopenia (unusually low platelet count), anasarca (swelling of multiple tissues or organs), fever, reticulin fibrosis or myelofibrosis (bone marrow disease or cancer) and organomegaly (enlargement of any organs).2,5 This subtype generally has more severe complications than iMCD without TAFRO.
- Idiopathic multicentric Castleman disease-not otherwise specified (iMCD-NOS)
This includes all individuals with iMCD without TAFRO. The disease generally involves less severe symptoms.2,4 A subset of individuals with iMCD-NOS have chronic thrombocytosis (high levels of platelets) and hypergammaglobulinemia (high levels of antibodies). This is sometimes refered to as idiopatic multicentric Castlman disease with plasmacytic lymphadenopathy (iMCD-IPL).6,7
Please speak to your medical team to learn more about the symptoms and complications of the different subtypes of iMCD.
Disability Impacts
Rare diseases are often serious and progressive, exhibiting a high degree of symptom complexity, leading to significant disability. Majority of the estimated two million Australians living with a rare disease meet the Australian Government’s definition for disability (in accordance to the Australian Public Service Commission and Australian Bureau of Statistics), and many experience severe and permanent disability impacts. If you or someone you care for is experiencing disability-related impacts from a rare condition, please speak with a health or disability professional for advice. Information about relevant disability support can be found at the RARE Portal’s Disability Support Information page.
Cause and Inheritance
The cause of iMCD is unknown.1 There are no known risk factors.
Diagnosis
Diagnosis of iMCD may be made based on the results of an excisional lymph node biopsy and blood and urine tests.4,9 An excisional lymph node biopsy involves the removal of an entire lymph node (either under local anaesthetic while you are awake or general aesthetic while you are asleep). The lymph node is then examined under a microscope to look for characteristic signs of Castleman disease.
Blood and urine tests may also be performed look for other signs of iMCD such as:4,5,8
- anaemia (low amount of red blood cells)
- high inflammatory markers in blood (such as CRP and/or ESR)
- protein and blood cells in urine which can indicate kidney disease
- high number of platelets (clotting agent in blood)
- high globulins and low albumin levels in blood
- high levels of plasma cells in bone marrow and lymph nodes
A differential diagnosis can rule out other conditions with similar symptoms, such as Unicentric Castleman disease, KSHV/HVV-8-associated Castleman disease, POEMS syndrome, Hodgkin lymphoma, non-Hodgkin lymphoma, Systemic lupus erythematous, Rheumatoid arthritis and other autoimmune diseases, and acute viral infections including EBV and HIV infection.2,4,5,8-10
Please speak to your medical team to learn more about the available diagnostic pathways for iMCD.
Treatment
There is currently no curative treatment for iMCD. Treatment is targeted at managing symptoms (symptomatic management) and involves a multidisciplinary care team.4,5,8 This may include biologic medications which can reduce inflammation. In some cases where the symptoms are severe and/or don’t respond to biologic medications, corticosteroids and/or chemotherapy may be used. Other types of medications may also be used to treat complications on a case-by-case basis.
Please speak to your medical team to learn more about the possible treatment or management options for your condition. Treatment will depend on an individual’s specific condition and symptoms. It is also important to stay connected to your medical team so that you can be made aware of any upcoming clinical trial opportunities.
Clinical Care Team
Healthcare professionals involved in the treatment of iMCD may include general practitioners (GP), paediatricians, haematologists, pulmonologist, nephrologists and oncologists.2,8,11 The need for different healthcare professionals may change over a person’s lifetime and extend beyond those listed here.
Clinical care for rare diseases often involves a multidisciplinary team of medical, care and support professionals. Please note that the information provided here is as a guide and that RVA does not necessarily monitor or endorse specific clinics or health experts.
For many rare diseases, palliative care services may be relevant and useful. Palliative care services are available for people (adults, children and their families) living with a life-limiting illness. Palliative care services provide assistance, support, resources and tools to help people manage their illness and the symptoms, ease pain, and improve comfort and quality of life. Palliative care is not only for end-of-life care. It can also help at any stage of illness from diagnosis onwards, and will look different for different people. For more information about palliative care and how it can help you, please visit:
Clinical Care Guidelines
We are not aware of any clinical care guidelines for iMCD in Australia. If you know of any relevant care guidelines, please let us know via the Contribute page.
The following guidance is available from international experts outside Australia; however, there may be information that is not relevant or applicable to the Australian context, and may not be up to date:
- The management of Castleman disease – a ‘Good Practice Paper’ containing recommendations where there is limited evidence but a degree of consensus or uniformity is likely to be beneficial to patient care; compiled according to the British Society for Haematology (BSH) process and published in 2021
- International, evidence-based consensus diagnostic criteria for HHV-8–negative/idiopathic multicentric Castleman disease(iMCD); published in 2016 by a working group of 34 experts in iMCD and related disorders from 8 countries (including 2 physicians that are also iMCD patients)
- International, evidence-based consensus treatment guidelines for idiopathic multicentric Castleman disease (iMCD) was established in 2018 by a working group of 42 experts in iMCD and related disorders from 10 countries;
- the effectiveness of the practices recommended in these guidelines has since been evaluated in a trial and reported in a 2023 publication, “Treatment consistent with idiopathic multicentric Castleman disease guidelines is associated with improved outcomes.”
Emergency Management
Individuals living with rare diseases may have complex medical issues and disabilities, which are not always visible. It is often useful to refer to their medical history as well as personal information such as a medical card, doctor’s letter, or if available, a rare disease passport, for relevant information.
Research
Castleman Disease Collaborative Network: Physicians & Researchers has information on relevant research and resources for Castleman disease.
There are specific considerations around participating in rare disease research, including clinical trials. It is important to be mindful of issues such as data privacy, research ethics, consent and differences in research regulations between Australia and other countries.
If you are interested in finding clinical trials for your condition, please visit the following websites; however, there may not be any clinical trials available:
It is best to discuss your interest in any clinical trials with your medical team to determine suitability and eligibility.
Rare Disease Organisation(s)
There are currently no known organisations for Castleman disease in Australia. If you are aware of any Castleman disease organisations in Australia, please let us know via the Contribute page. If you are interested in starting an Australian organisation, please see Engaged, Ethical and Effective: A Guide for Rare Disease Organisation Leaders in Australia.
Please note that RVA does not monitor or endorse each group/organisation’s operational governance and activities. When engaging with a group, please consider the information on the RARE Portal’s Finding Helpful Peer and Community Supports page.
Lived Experience
iMCD varies between individuals, and each person’s experience is unique.
If you would like to share your personal story with RVA, please visit the Rare Voices Australia: Share Your Story page. RVA will consider your story for publishing on our website and inclusion on the RARE Portal.
Support Services and Resources
For information on available government and social services that provide support for individuals with a rare disease, please visit the National and State Services pages.
Mental Health
People living with a rare disease, including families and carers, often face unique challenges such as diagnostic delays, misdiagnoses, limited treatment options, and limited access to rare disease specialists and support. These challenges may impact people’s emotional wellbeing and quality of life. Many people find it helpful to seek mental health and wellbeing support to cope with ongoing stress and uncertainty. Connecting with people who have shared experiences through a support group may also be helpful. Information about relevant mental health and wellbeing support can be found at:
- Mental Health and Wellbeing Support for Australians Living with a Rare Disease
- The National and State Services pages underneath the ‘Mental Health’ sections listed
Other Information
Further information on Castleman disease can be found at
Useful Links for Healthcare Professionals
References
- National Organization for Rare Diseases. Castleman Disease. Published 1988-2022. Updated 16 June 2022. Accessed 21 August 2024. https://rarediseases.org/rare-diseases/castlemans-disease
- Castleman Disease Collaborative Network. About Castleman Disease. Accessed 10 August 2024. https://cdcn.org/castleman-disease/
- Orphanet. Castleman disease. Accessed 20 August 2024. https://www.orpha.net/en/disease/detail/160
- Fajgenbaum DC, Uldrick TS, Bagg A, et al. International, evidence-based consensus diagnostic criteria for HHV-8–negative/idiopathic multicentric Castleman disease. Blood. 2017;129(12):1646-57. https://doi.org/10.1182/blood-2016-10-746933
- Carbone A, Borok M, Damania B, et al. Castleman disease. Nature Reviews Disease Primers. 2021;7(1):84. https://doi.org/10.1038/s41572-021-00317-7
- Gao Y-h, Liu Y-t, Zhang M-y, et al. Idiopathic multicentric Castleman disease (iMCD)-idiopathic plasmacytic lymphadenopathy: A distinct subtype of iMCD-not otherwise specified with different clinical features and better survival. British Journal of Haematology. 2024;204(5):1830-7. https://doi.org/10.1111/bjh.19334
- Nishikori A, Nishimura MF, Nishimura Y, et al. Idiopathic Plasmacytic Lymphadenopathy Forms an Independent Subtype of Idiopathic Multicentric Castleman Disease. Int J Mol Sci. 2022;23(18). https://doi.org/10.3390/ijms231810301
- Lomas OC, Streetly M, Pratt G, Cavet J, Royston D, Schey S, et al. The management of Castleman disease. British Journal of Haematology. 2021;195(3):328-37. https://doi.org/10.1111/bjh.17688
- van Rhee F, Oksenhendler E, Srkalovic G, Voorhees P, Lim M, Dispenzieri A, et al. International evidence-based consensus diagnostic and treatment guidelines for unicentric Castleman disease. Blood Advances. 2020;4(23):6039-50. https://doi.org/10.1182/bloodadvances.2020003334
- National Organization for Rare Disorders. POEMS Syndrome. Published 1991-2021. Updated 23 September 2021. Accessed 22 August 2024. https://rarediseases.org/rare-diseases/poems-syndrome/
- Genetic and Rare Disease Information Centre. Castleman Disease. Updated July 2024. Accessed 21 August 2024. https://rarediseases.info.nih.gov/diseases/12656/castleman-disease
Contributors
This page has been developed by Rare Voices Australia (RVA)’s RARE Portal team.
If you are aware of any additional information that may benefit stakeholders with an interest in this page, or if you notice any broken links or inaccurate information, please let us know via the Contribute page.

